Author: Anne Holland, CEO and Founder
A few weeks ago, I moderated a panel discussion for the Texas Medical Device Alliance on the topic of medical device packaging and validation.
The webinar was intended to help startups and other medical device manufacturers understand the nuances and complexities of packaging their products in compliance with regulatory requirements.
Highlighted below are the key takeaways from our informative discussion:
- Get to know ISO 11607
- Test for the worst-case scenario
- Learn best practices from industry experts
Similar to other stages of bringing your medical device to market safely and efficiently, it’s never too early to think about the quality and regulatory requirements for packaging.
If you haven’t thought about the interaction between your device and how it will be packaged, sealed, and sterilized, before reaching its end-user, don’t delay.
ISO 11607 the Standard for Packaging Sterile Medical Devices
Before you make any packaging decisions, it’s essential that you understand the basics of ISO 11607.
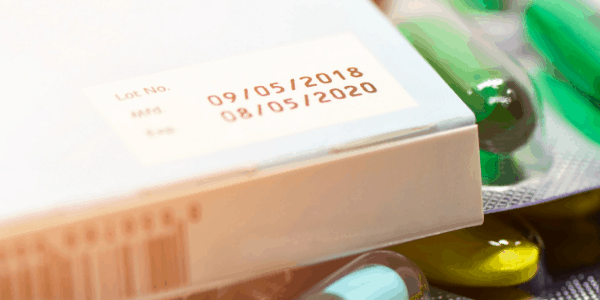
ISO 11607-1:2019 – Packaging for terminally sterilized medical devices – Part 1:Requirements for materials, sterile barrier systems and packaging systems specifies the requirements and testing methods for materials and packaging systems that maintain the sterility of a product until the point of use.
The spirit of this standard is to ensure the packaging protects the device so that it remains sterile until it is ready for use. The life of the packaging must match or exceed that of the product.
This product development phase requires cross-departmental input from the product design, logistics, marketing, and quality teams.
While ISO 11607 applies to sterile medical devices, the spirit of delivering a device protected from the elements so that it works as intended when it arrives in the hands of the end-user is a universal need.
Testing for the Worst-Case Scenario
Baseline testing to validate medical device packaging evaluates three components:
- Package strength
- Package integrity
- Potential for microbial contamination
The safest path is to test for the worst-case scenario. If your device packaging meets the testing requirements in the most extreme cases, it will likely hold-up under more moderate conditions, and you’ll have the testing results to back you up.
Pro-tip: baseline testing using accelerated aging of your product alongside a real-time aging comparison must be started within three months of each other.
Medical Device Packaging Best Practices
We also discussed some of the common questions that we regularly hear from our clients related to packaging.
For startups and those new to the medical device industry, understanding potential risks and planning for scenarios experienced by your peers can help you get ahead of the game.
Here’s a sample of the questions we discussed:
- What to look for in a contract packager
- When to repeat validation if there’s a change in packaging
- How to leverage pre-validated packaging elements
Listen to a recording of the webinar for highlights from the panelist’s responses to my questions.
Lean Into Our Medical Device Packaging Expertise
When you look behind the curtain, there’s a lot to understand about the safe packaging of medical devices.
Startups and those bringing a new product to market should consider partnering with trained experts.
Our unique blend of medical device microbiology and sterilization expertise combined with our decades of bringing devices to market safely can help your company find the right packaging solution.
Contact us today to talk to a medical device packaging expert!
Thank you to the participants on the webinar panel:
Dana Wilcox, CEO of Mainstream Medical Devices, LLC
Andy Fronk, Principal Consultant of Bear Creek Consulting
Andrew Cockerham, Director of Quality, Alafair Biosciences, Inc.
Jennifer Gygi, B.S., SM (NRCM) Packaging Expert, Nelson Labs